Novel and Emerging Technologies (NET) Grant
Professor Ruth Andrew, University of Edinburgh
Amount: £249,773

Summary: Coronary heart disease (CHD) is one of the single biggest killers in the UK and worldwide. In CHD, fat builds up the blood vessels forming so called “plaques”. If these plaques break up or burst, they can cause blood clots, leading to a heart attack or stroke. It has been found that a sticky molecule called Lipoprotein a (Lp(a)) affects how likely a plaque is to break up. Professor Andrew and her team will be using mass spectrometry imaging to determine how this molecule is distributed within plaques and how it affects their likelihood to break up. This will not only inform our understanding of plaques in coronary heart disease but also provide potential therapeutic targets for early treatment.
Coronary heart disease (CHD) is a leading cause of death and disability worldwide. It can be caused by fat building up in blood vessels, so-called “plaque”. Plaques can narrow and harden the blood vessels and reduce blood and oxygen flow to major organs causing damage. Plaques can also break off, causing blood clots, or become unstable and burst. The broken pieces, “clots”, block blood vessels and prevent blood flow. If this occurs in a coronary artery (a blood vessel that provides blood and oxygen to the heart) this can cause a heart attack and potentially death.
There are a number of drug treatments that are used to stop plaques from forming but they do not work for everybody. It has recently been discovered that high levels of a “sticky” protein called lipoprotein(a) (commonly called Lp(a)) in the blood strongly predict the likelihood of plaques becoming unstable. Whether or not someone has high levels of Lp(a) is determined by their genes, rather than diet or other lifestyle factors.
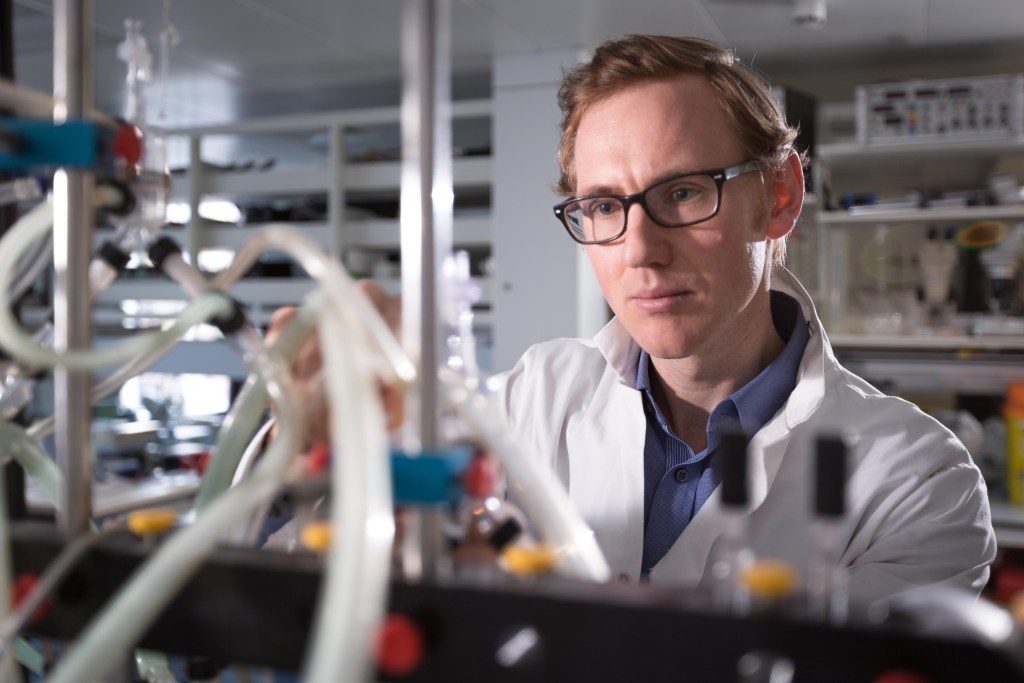
Professor Andrew and her team at the University of Edinburgh will investigate how high Lp(a) levels in blood contribute to plaque instability by studying plaques taken from patients during surgery. Using a technology called “mass spectrometry imaging”, they will map how Lp(a) is distributed in plaques and find out what damage it causes. For example, areas of plaques with high Lp(a) in specific regions might be more likely to burst. The information gained will increase understanding about how certain molecules affect the plaque shape and structure. The team’s findings will potentially reveal more about Lp(a) and its link with plaque development, supporting clinicians to diagnose heart disease by working out better ways to screen at-risk patients and treat them earlier.
This will mean that coronary heart disease can be caught in patients before they know they have heart problems and slow or stop plaque building up. This will extend the period of life when individuals can benefit from good health and its life benefits. This information will also help pharmaceutical companies both design more effective drugs for lowering Lp(a) and understand which patients respond best to treatments.